48 year old with complaints of VOMITINGS ,loose stools ,SOB
45 Year old male came with chief complaints of vomitings,loose stools,sob since morning
On presentation patient tachypneic with hypoxia with BP 80/50 mm hg with distended abdomen and pedal oedema
Vomitings - bilious ,non projectile ,water as content
Loose stools - watery stools ,small in volume ,Malena present associated with epigastric pain
SOB grade 4 since morning . No chest pain ,palpitations ,giddiness ,sweating
No h/o fever ,cold,cough,burning micturition
Personal history -
appetite- lost
Diet -veg
alcohol intake last 1 month back
PHYSICAL EXAMINATION -
No pallor /icterus/cyanosis/clubbing /oedema /lymphadenopathy
Dehydration - present
Temperature - afebrile
PR - 112 bpm /min
RR - 32 cpm
BP - 90/50
Spo2 room air - 88
Grbs - 137mg /dl
SYSTEMIC EXAMINATION
CVS - S1,S2 heard
Respiratory - no dyspnea ,decreased breath sounds ,
ABDOMEN -
Shape of abdomen - distended(fluid thrill )
Tenderness -no
Hernial orifices -normal
Free fluid - yes ,fluid thrill present
Genitals - scrotal swelling positive
CNS - Level of consciousness - drowsy
Speech - normal ( at the time of admission)
Glasgow Coma scale - E4V3M3
He came to casualty before with complaints of b/l pedal oedema and abdominal distension
INVESTIGATIONS
Rapid test for covid negative
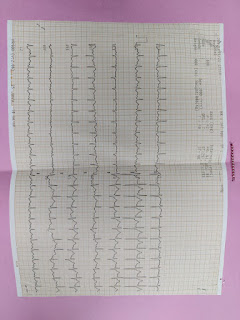
ECG
CHEST X RAY AP VIEW
ABG
RFT
LFT
Around 6 pm patient had bouts of vomitings followed by sudden cardiac arrest with absent central and peripheral pulses with falling saturations
Positive cycles of cpr done ,received intubated with ET -7mm ,pre and post intubation secretions are aspirations ,active bleed + about 50 ml
Post intubation vitals are
Bp -100(sbp)
PR-98 bpm
Spo2-94 % at room air
Temperature - afebrile
Post intubation pt was started on inotropes and connected to mechanical ventilation
CVS - s1,s2 heard
R/s - b/l crepts in IAA,IMA,ISA
P/A - distended ,visible veins ,fluid thrills positive
PROVISIONAL DIAGNOSIS - CHRONIC LIVER DISEASE WITH OESOPHAGEAL VARICES
Treatment given - BEFORE INTUBATION
1)Head end elevation
2)O 2 inhalation to maintain spo2 > 94
3)TAB LASIX 40 MG PO/BD
4)TAB ALDACTONE 50 MG PO/OD
5)TAB.PROPANOLOL 20MG PO/OD
6)INJ.PANTOP 40 MG IV/BD
7)INJ ZOFER 4 MG IV/SOS
8)MONITOR VITALS - 4 TH HRLY
9)GRBS - 6 TH HRLY
10)I/O ,WEIGHT,ABDOMINAL GIRTH -CHARTING
AFTER INTUBATION
1)head end elevation
2)RT feeds 50 ml 2 no hourly (water),100ml 4 TH hourly (milk protein powder )
3)INJ PANTOP 40 MG IV/BD
4)INJ ZOFER 4 MG IV/BD
5)INJ NORAD 2 AMP IN 48 ML NS @16ML/HR (TO MAINTAIN MAP 55 TO 60 %)
6)INJ DOBUTAMINE 1 AMP IN 45 ML NS @ 3.5ML/HR
7)INJ TRANEXA IV stat
8)INJ LASIX INFUSION @5MG/HR
9)MECHANICAL VENTILATOR
10)I/O ,TEMP CHARTING
11)Monitor vitals 4 hourly
Death summary
48-year-old male came to casualty with vomitings,loose stools and shortness of breath ,on presentation patient drowsy but arousable with spo2 88 at RA with hypotension
patient was put on oxygen mask with supportive care. At around 4:30 PM on
6/12 /2021 had sudden onset of profuse vomiting with sudden cardiac arrest, CPR done six cycles and intubated with ET -7mm and connected to mechanical ventilator ( ACMV-VC)
In view of hypotension,patient was started on ionotropes and monitored vitals and serial abg were done .even on ionotropes ,patient BP could not be improved, had cardiac arrest at 5 25 am on 7/12/21 with absent central and peripheral pulses with dilated pupils .CPR initiated and continued for 6 cycles .in spite of all the efforts,patient could not be revived and declared dead on 7/12/21 at 5 53 am with ecg showing no electrical activity
Immediate cause :refractory hypotension and refractory metabolic acidosis (Post -cpr status )
Antecedent cause :chronic liver disease with grade 3 oesophageal varices with right heart failure







Comments
Post a Comment